October bimonthly assessment exam
I)57 year old man with jaundice, pedal edema and abdominal distension since three years and bleeding gums since three days"
https://swathibogari158.blogspot.com/2020/09/chronic-decompensated-liver-disease.html
1) What is the reason for this patient's ascites?
A) Chronic alcoholic ---> Chronic liver disease --->Decreased liver function---> Hypoalbuminemia---> Ascites
Albumin is synthesized in the liver, and low serum albumin can be indicative of liver failure or diseases such as cirrhosis as seen in our patient. So as liver is failing it's function of protein production is coming down too.
Hypoalbuminemia decreases the total protein concentration in blood plasma, also known as the colloid osmotic pressure, which causes fluid to exit the blood vessels into tissues to equalize the concentrations. This leads to build-up of fluid in the abdomen known as ascites.
The production of lymph increases in cirrhosis with portal hypertension as a result of an elevated pressure in the sinusoids. When the production of lymph exceeds the capacity of the lymphatic system, ascites results.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4992465/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3701854/
2) Why did the patient develop bipedal lymphedema? What was the reason for the recurrent blebs and ulcerations and cellulitis in his lower limbs?
A) As there is lymphatic blockage, poor drainage of lymph leads to bipedal lymphadema.
Chronic lymphatic blockage and venous stasis causes the cellulitis in the dry fissured skin
Also as the patient isn't taking proper aseptic precautions, not doing frequent dressing of his wounds plus abuse of steroids as said in history there is poor skin hygiene resulting in recurrent blebs, ulcerations (poor wound healing) and cellulitis. These are recurring also because of poor wound healing due to severe anemia and hypoalbuminemia
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6303460
3) What was the reason for his asterixis and constructional apraxia and what was done by the treating team to address that?
A) Asterixis has occured because patient has developed hepatic encephalopathy.
Some investigators contend that hepatic encephalopathy is a disorder of astrocyte function. It is theorized that neurotoxic substances, including ammonia and manganese, may gain entry into the brain in the setting of liver failure. These neurotoxic substances may then contribute to morphologic changes in the astrocytes.
Second reason is hyperammonemia. Two factors contribute to the hyperammonemia that is seen in cirrhosis. First, there is a decrease in the mass of functioning hepatocytes, resulting in fewer opportunities for ammonia to be detoxified by the above processes. Secondly, portosystemic shunting may divert ammonia-containing blood away from the liver to the systemic circulation.
https://emedicine.medscape.com/article/186101-overview#a2
The treating team gave
a) Syp lactulose 15ml/PO/TID
Lactulose Lactulose is the most frequently utilized agent in the treatment of hepatic encephalopathy because of its efficacy and the fact that it has few serious side effects. When the intestinal flora metabolized lactulose, bacterial incorporation of nitrogen increases as does the bacterial mass. The presence of a carbohydrate and the acidic environment caused by the production of organic acids also act to reduce the breakdown of other nitrogen-containing compounds to ammonia and other potential cerebral toxins
https://pubmed.ncbi.nlm.nih.gov/8872452
b) Syrup Hepamerz
LOLA (Hepa-merz) is a stable salt of the two constituent amino acids. L-ornithine stimulates the urea cycle, with resulting loss of ammonia. Both l-ornithine and l-aspartate are substrates for glutamate transaminase. Their administration results in increased glutamate levels. Ammonia is subsequently used in the conversion of glutamate to glutamine by glutamine synthetase.
https://www.medscape.com/answers/186101-25734
c) Tab Rifamixin
Rifaximin is a poorly absorbed antibiotic that is thought to reduce ammonia production by eliminating ammonia-producing colonic bacteria.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3105611
4) What was the efficacy of each treatment intervention used for this patient? Identify the over and under diagnosis and over and under treatment issues in the management of this patient.
A) Efficacy of each treatment is mentioned below
1. Air or water bed to prevent pressure bed sores in the dependent areas
2. Fluid restriction <1.5litres/day so as to decrease of fluid dissemination into the extra vascular space
Salt restriction <2.4gms/day to prevent retention of water due to osmotic gradient as sodium causes retention
3. Inj augmentin 1.2gm IV/BD to prevent secondary bacterial infections
4. Inj Pantoprazole 40 mg IV/OD
the use of this class of drugs seems more habit related than evidence-based eventually leading to an increase in health costs.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2712162/
5. Inj zofer 4mg IV/BD
6. Tab lasilactone (20/50)mg BD ( combination of furosemide and aldactone to decrease pedal oedema
If SBP <90mmhg - to avoid excessive loss of fluid
Use of this drug must be done carefully
Diuretic therapy: Decreased serum potassium levels and alkalosis may facilitate the conversion of NH4+ to NH3. At the author’s institution, diuretic-induced hypovolemia is the most common reason for patients with previously well-controlled hepatic encephalopathy to present to the emergency room with worsening mental function.
https://emedicine.medscape.com/article/186101-overview#a6
7. Inj vit k 10mg IM/ STAT ( as vitamin K causes coagulation to further prevent bleeding manifestions
8. Syp lactulose 15ml/PO/BD for hepatic encephalopathy
In patients with minimal hepatic encephalopathy, lactulose was more effective than placebo in terms of improving patient performance on psychometric testing.
https://emedicine.medscape.com/article/186101-overview#a7
9. Tab udiliv 300mg/PO/BD contain ursodeoxycholic acid and is currently the only established drug for the treatment of chronic cholestatic liver diseases. It has cytoprotective, anti-apoptotic, membrane stabilizing, anti-oxidative and immunomodulatory effects
10.Syp Hepamerz 15 ml/PO/OD
This drug is aptly used as we have evidence of the same ( above answer)
https://www.medscape.com/answers/186101-25734
11.IVF 1 NS slowly at 30ml/hr to maintain hydration
12. Inj thiamine 100mg in 100mlNS /IV/TID as thiamine deficiency's occur in chronic alcoholics
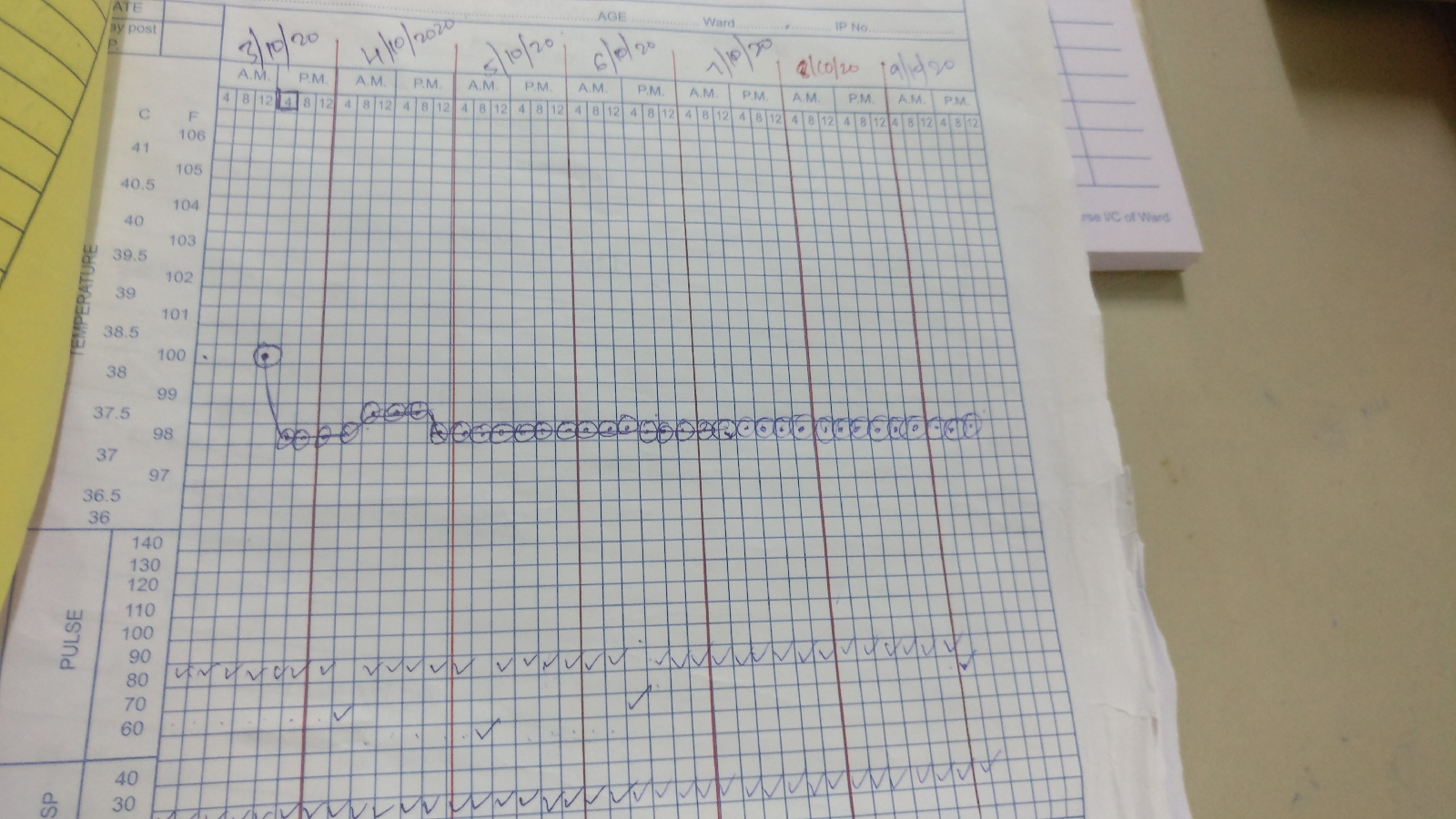
13.strict BP/PR/TEMP/Spo2 CHARTING HOURLY
14.strict I/O charting
15.GRBS 6th hourly
16.protein x powder in glass of milk TID for protein supplementation and muscle wasting which commonly occurs in cirrhosis patients
17. 2FFP and 1PRBC transfusion to support coagulation pathways and improve the patient's HB levels as he is in severe anemia
18 .ASD done for wound infections and ulcer
19. High protein diet (2eggs / day) for decreased albumin synthesis
19 Inj metrogyl 500mg IV/TID to prevent anerobic infections
20. Tab rifaximin 550mg BD for 3days
Multiple clinical trials have demonstrated that rifaximin at a dose of 400 mg taken orally 3 times a day was as effective as lactulose or lactitol at improving hepatic encephalopathy symptoms. Similarly, rifaximin was as effective as neomycin and paromomycin. Rifaximin had a tolerability profile comparable to placebo. It was better tolerated than both the cathartics and the other nonabsorbable antibiotics. A potential mechanism for rifaximin's clinical activity is its effects on the metabolic function of the gut microbiota, rather than a change in the relative bacterial abundance.
https://emedicine.medscape.com/article/186101
https://www.medscape.com/answers/186101-25744
II) A 54 year old male with cough,abdominal tightness,pedal edema and diarrhea.
https://sainiharika469.blogspot.com/2020/09/hello-everyone.html?m=1
1) Why were his antitubercular therapy stopped soon after his current admission? Was he symptomatic for ATT induced hepatitis? Was the method planned for restarting antitubercular therapy after a gap of few days appropriate? What evidence is this approach supported by?
A) Among the first-line quadruple therapy drugs (INH, RMP, PZA, and EMB), INH, RMP, and PZA are metabolized mainly by the liver, and therefore, are potentially hepatotoxic. And as the patient was already showing deranged LFTS, the treatment must have been stopped.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5366108/
This article is the evidence for att drug induced liver injury with underlying precipitating factors like, pt's weight, raised alk phosphatase levels and chronic alcoholic. So stopping the drug to reconfirm the cause of hepatitis and restarting with ethambutol and streptomycin, which are less hepatotoxic seems to be a good approach. Then restarting one of 3 hepatoxic drugs with Minimum dose and start increasing it.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3940527/
2) What were the investigational findings confirming the diagnosis of pulmonary TB in this man?
A) Sputum positive TB with RIFAMPICIN sensitivity
Bilateral Infiltrates in chest x-ray
Plueral thickening and fibrocavitory changes noted in HRCT.
Also typical clinical history suggestive of pulmonary TB- low grade fever, cough with expectorant and weight loss.
3) What was the cause of his ascites?
A) Chronic alcoholic ---> Chronic liver disease --->Decreased liver function---> Hypoalbuminemia---> Ascites
Chronic alcoholic---> Alcoholic liver disease---->
Portal hypertension---> Ascites
( Ascitic fluid analysis- high SAAG)
4) What are the efficacy of each intervention mentioned in his treatment plan and identify the over and under diagnosis as well as over and under treatment issues in it.
A)
Inj Human Actrapid Insulin s/c 8am - 2pm - 8pm
Known diabetic since 8 years so for sugars control
Inj Pantoprazole 40 mg IV/OD
Inj optineuron 1 amp in 100 ml NS Iv/bd nutritional supplements (Vit B12)
ATT to be with held
Syp lactulose 15ml HS prophylactic to prevent hepatic encephalopathy
Protein powder 3 to 4 scoops in 1 glass of milk or water QID for protein supplementation
Stop all OHA s higher risk of ot going into hypoglycemia
Grbs charting 6th hrly
Strict I/0 charting
High protein diet 4eggs daily for Protein supplementation
ORS sachets in 1 litre of water because patient had diarrhea So to compensate the lost electrolytes
Bp charting hourly
Inj PIPTAZ 4.5gm/IV/bd stat as an antibiotic coverage
But it can be avoided because patient is diagnosed with pulm tb (other antibiotics in regimen) plus diarrhea doesn't require such a strong antibiotic
Vit k 10 mg Iv OD for 5 days prevent forthcoming bleeding manifestations as his PT INR APTT are elevated
Temp BP PR monitoring 4th hourly
IVF - 1 DNS @50ml/hr since loss due to diarrhea
Nebulisation with salbutamol and mucomist 12th hourly for cough
Inj thiamine 100 mg in 100 ml NS IV TID as it's deficiency is common in chronic alcoholics
III) 47 year old man with bipedal edema since one year and abdominal distension since one month
https://sushma29.blogspot.com/2020/09/ascites-secondary-to-nephrotic-syndrome.html?m=1
1) What will be your further approach toward managing this patient of nephrotic syndrome? How will you establish the cause for his nephrotic syndrome?
A) Start patient in ARBS or ACE inhibitors and low dose steroids and also statins
Next would be finding out the cause of nephrotic syndrome to treat him better
Common primary causes of nephrotic syndrome include kidney diseases such as minimal-change nephropathy, membranous nephropathy, and focal glomerulosclerosis.
Secondary causes include systemic diseases such as diabetes mellitus, lupus erythematosus, and amyloidosis
https://www.medscape.com/answers/244631-154722
Primary (idiopathic) forms:
-Minimal change disease - but seen in children so ruled out .
-Focal segmental glomerulosclerosis- seen in adults so a possibility
-Membranous nephropathy - Most commonly seen in adults ,so a possibility.( Anti PLA2R antibodies)
B) Secondary forms :
-Diabetic nephropathy- pt not a known diabetic
-Amyloid nephropathy: can be associated with multiple myeloma (AL amyloidosis) or chronic inflammatory disease such as rheumatoid arthritis (AA amyloidosis) - not seen in our pt.
-Lupus nephritis. - not a possibility
- HIV HBsAg were negative . No features of STD .
- Malignancy - lung , adenocarcinoma of colon , stomach , prostate carcinoma ,non hodgkins lymphoma all these are secondary causes of nephrotic syndrome - which could be a possibility in this patient owing to chronic weight loss and muscle wasting and loss of appetite.
-Can search for primary focus of malignancy ,
By doing HRCT CT abdomen, endoscopy/ colonoscopy but as these done later as they are more expensive so renal biospy is suggested before them
2) What are the pros and cons of getting a renal biopsy for him? Will it really meet his actual requirements that can put him on the road to recovery?
A) Because in our patient common secondary causes are eliminated, we can think of renal biopsy.
Adult nephrotic syndrome of unknown origin may require a renal biopsy for diagnosis. Reaching a pathological diagnosis is important because minimal-change disease, focal glomerulosclerosis, and membranous nephropathy have different treatment options and prognoses. It is important to differentiate minimal-change disease presenting in adults from focal glomerulosclerosis, as the former has an excellent response to steroids. Another entity called immunoglobulin M (IgM) nephropathy falls in between the two and has an intermediate response to steroids.
https://www.medscape.com/answers/244631-154752
https://academic.oup.com/ndt/article/30/4/528/2332871
Pros of renal biospy
We have higher chances of getting to the cause of nephrotic syndrome thus helping us in better management of patient
Cons of renal biospy
Time consuming and expensive
Most common complication is pain and bleeding at the biopsy site
Injury to surrounding tissues during procedure
Infections though rare are possible
https://emedicine.medscape.com/article/2093338-overview#a7