Fever, generalized weakness and loss of appetite since 10 days
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Case presentation:
30 year male patient, a construction labourer, came with the complaints of fever, generalized weakness and loss of appetite since 10 days.
Patient was apparently asymptomatic 10 days ago. Then he had high grade continuous fever, which temporarily relieved on medication. The fever was associated with chills and rigor, dry cough, generalized weakness and loss of appetite. Initially they want to RMP were he was prescribed paracetamol and diclofenac plus serratiopeptidase and also advised to take herbal medication too. He used these for 5 days twice daily. As his generalized weakness increased from the past 4 days, he came to our hostipal for futher evaluation.
It was not associated with pain abdomen, loose stools, vomitings, sore throat.
No h/o burning micturition, headache.
Past history
Not a K/c/o DM, HTN, asthma, TB, CAD, epilepsy.
Personal history
Mixed diet, decreased appetite, adequate sleep, regular bowel and bladder habits
Chronic alcoholic with daily consumption of 250ml of whiskey since 12 years
He consumes 2 cigarettes per day since 12 years
He consumes betel leaf occassionally
Family history
No K/c/o DM, HTN, asthma, TB, CAD, epilepsy
General examination
Patient is consicous coherent cooperative
Icterus +ve
No pallor clubbing cyanosis lymphadenopathy and odema
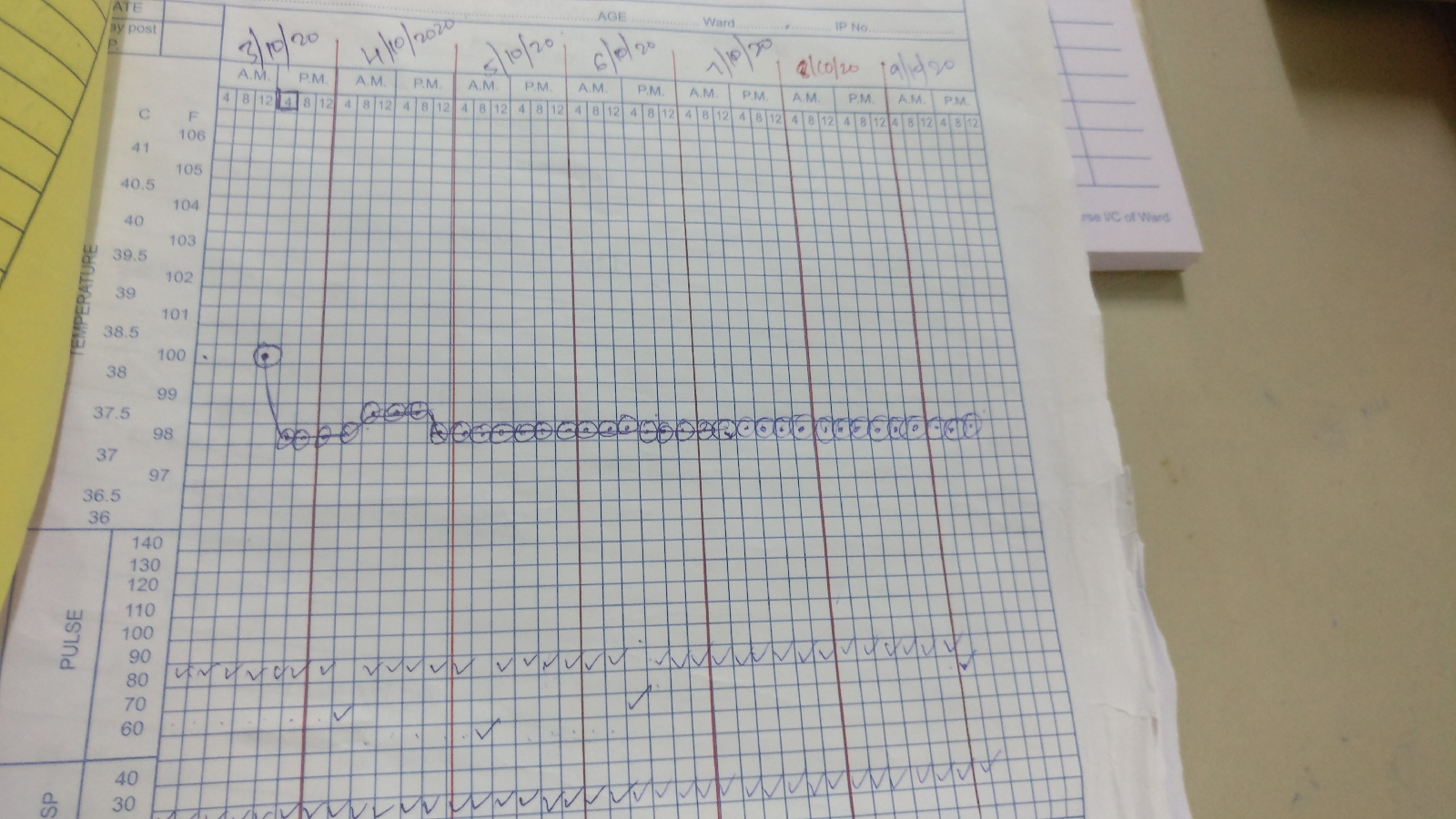
Temperature- 100.4F
Pulse- 56bpm with regular rate, rhythm and volume
BP- 90/70 mmHg recorded in right arm supine position
GRBS- 143mg/dl
RR - 18cpm
Systemic examination :
CVS
S1,S2 heard, no murmurs
RS
BAE present, normal vehicular breath sounds heard, no additional sounds were heard.
Per Abdomen:
All quadrants moving equally with respiration, no scars, sinuses and engorged veins
On palpation abdomen is soft, non- tender and no organomegaly
CNS:
GCS 15/15
Higher mental function- Normal
Cranial Nerve examination- Normal
Motor system examination
Tone- Normal
Power- UL normal
LL- Hip
Flexion_extension 5/5. 5/5
Lateral and medial rotation 5/5. 5/5
Abduction and adduction. 5/5. 5/5
Knee
Flexion and extension. 5/5. 5/5
Ankle
Dorsi and plantar flexion. 5/5 5/5
Inversion and eversion. 5/5 5/5
Reflexes- Superficial Normal
Deep Normal
Sensory system examination- Normal
Gait- Antalgic gait
Cerebellar examination- Normal
Investigations
Day 1 3rd October 2020
Day 2 4th October 2020
Day 3 5th October
Day 5 7th October
Treatment
IVF NS @100 ml/hr continous
Inj Pantoprazole 40mg IV OD
Tab Udiliv 150mg PO BD
Temperature charting 4th hrly
Inj Optineuron 1amp in 100ml NS IV OD
GRBS 8th hrly
I/O Charting
After neurology referral for burning sensation and severe leg pains, he was prescribed
Tab ACECLOFENAC BD
TAB PREDNISALONE 20mg BD